COVID-19 vaccines and allergic reactions
In a major public health victory, vaccines for COVID-19 have now been developed, tested, and granted Emergency Use Authorization (EUA) by the Food and Drug Administration (FDA). This means that the FDA is allowing an unapproved medical product or unapproved use of an approved medical product to be used in an emergency public health situation because there is no adequate, approved or available alternative.
Even though these vaccines are authorized through an EUA, the FDA still considers them to be safe since the same rigorous phase three testing is necessary to show that they meet standards of both efficacy and safety. In studies, both vaccines have shown greater than 90 percent efficacy in a diverse population of more than 70,000 participants.
The two authorized vaccines
- Pfizer-BioNTech – Granted EUA status on December 11, 2020, for patients 16 years of age and older, given in two injections three weeks apart; and
- Moderna – Granted EUA status on December 18, 2020, for patients 18 years of age and older, given in two injections spaced four weeks apart.
Both of these vaccines are known as mRNA vaccines – containing messenger RNA, a nucleic acid that contains genetic material that helps the body form an immune response through a small amount of the viral protein on the mRNA that is delivered to the body with instructions on how to make proteins found in the virus.
The immune system then makes antibodies to this protein because it is recognized as foreign, and if the immune system encounters the COVID-19 virus, these antibodies and other immune pathways will protect the body from infection. (Source: American Academy of Allergy, Asthma and Immunology)
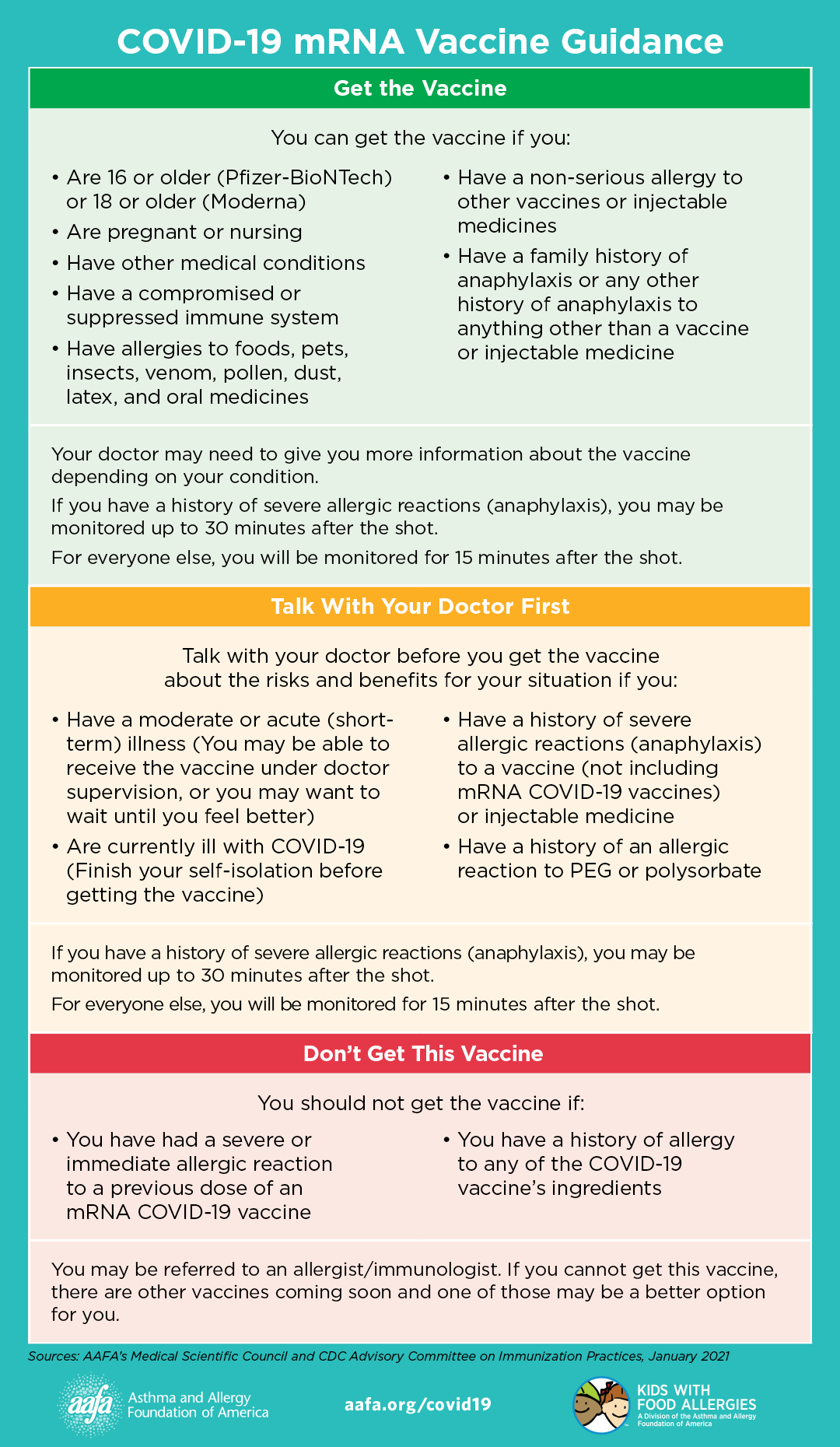
People who have allergies may not be more likely than the general public to have an allergic reaction to the vaccines, and if there are any concerns then talking to a healthcare provider about the benefits versus the risks may be worth considering.
People who receive the vaccine may experience pain, swelling or skin rash at the injection site and some swelling of the lymph nodes on the same side as the vaccinated arm, as well as systemic post-vaccination symptoms, which may include fever, fatigue, headache, chills, muscle or joint pain and/or inflammation. It is important to note that these are side effects, and may not be related to an allergic reaction. These symptoms can be delayed, occurring hours or days later and they are generally resolved within a few days.
While there have been stories in the news about people having allergic reactions to the Pfizer BioNTech vaccine, allergy groups advise that these severe reactions to any vaccine are always a possibility but they are rare. Additionally, people who are allergic to food, pets, insects, venom, pollen, dust, latex, and medicines can safely get the vaccine (source: CDC). It is also important to note that the vaccines do not contain food, latex or preservatives.
Preparing for post-vaccine allergic reactions
According to the American College of Allergy, Asthma, and Immunology, anaphylaxis rates are reported to be 5 per million with Pfizer-BioNTech and 2.5 per million with Moderna as of January 29, 2021.
The Centers for Disease Control and Prevention (CDC) provides recommendations for people who experience an allergic reaction after receiving a COVID-19 vaccination. It is important to note that since these recommendations are based on the current knowledge available at this time, they may evolve or change over time.
First, seek immediate medical attention. Vaccination sites are now requiring people with allergies to remain in a waiting area to ensure that there is no risk of a reaction. For people who are at the vaccination site when the allergic reaction occurs, staff can ensure that they receive the appropriate care that they need.
Reactions can be either severe or non-severe
- Severe allergic reactions or anaphylaxis may require treatment with epinephrine or EpiPen©or may require going to the hospital.
- Non-severe allergic reactions within four hours of receiving a COVID-19 vaccine may include hives, swelling, and/or wheezing.
People who have severe or immediate allergic reactions (hives, swelling, wheezing) or have questions related to the risk of an allergic reaction may want to reach out to a local board-certified allergist/immunologist.
A doctor can help determine if people who experience an allergic reaction to the first dose of a COVID-19 vaccine or experience allergic reactions to other types of vaccines can get safely vaccinated.
It is generally recommended that people who have had an allergic reaction to polyethylene glycol (PEG) or polysorbate should not get an mRNA COVID-19 vaccine.
Safeguards for allergic reactions
To help in anticipating allergic reactions in some people, the CDC provides recommendations for vaccination providers to help prepare for allergic reactions, which includes the following:
- Vaccinations should be administered in a healthcare setting and everyone who receives a COVID-19 vaccine should be monitored on site. People who have had severe allergic reactions or who have had any type of immediate allergic reaction to a vaccine or injectable therapy should be monitored for at least 30-minutes after getting the vaccine. All other people should be monitored for at least 15-minutes after getting the vaccine.
- Vaccination providers should have appropriate medications and equipment—such as epinephrine, antihistamines, stethoscopes, blood pressure cuffs, and timing devices to check your pulse—at all COVID-19 vaccination sites.
- For people who experience a severe allergic reaction after getting a COVID-19 vaccine, vaccination providers should provide rapid care and call for emergency medical services. You should continue to be monitored in a medical facility for at least several hours.
Learn more about what to expect after getting vaccinated for COVID-19, including normal side effects and tips to reduce pain or discomfort.
(Source: CDC)
Severe allergic reactions monitoring
Vaccination providers send a report of severe allergic reactions to the Vaccine Adverse Event Reporting System, which collects these reports from healthcare professionals, vaccine manufacturers, and the public. Studies are then conducted on reports of adverse events that are unexpected, appear to happen more often than expected, or have unusual patterns.
The American College of Allergy, Asthma and Immunology (ACAAI) COVID-19 Vaccine Task Force is also monitoring reporting on allergic reactions to the mRNA COVID-19 vaccines.
Experts are hopeful that many more vaccine candidates will be authorized in the near future, with different mechanisms and unique recommendations and safety data. As more of the population receives these vaccines, the number of cases will decline and more lives will be saved.
Amino acid-based formulas
Children with food allergies may benefit from an amino acid-based formula. By providing complete nutrition, these formulas designed for children over the age of 1 year, can fill in the gaps created by elimination diets or necessary food avoidance. EquaCare Jr. provides complete nutrition at a much lower price than comparable amino acid formulas and Essential Care Jr. provides a corn and soy free option with value-added ingredients at a similar price to other amino acid-based formulas. To learn more, call us at 1-833-377-2773.
Sources:
- https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/allergic-reaction.html
- https://acaai.org/news/acaai-provides-further-guidance-risk-allergic-reactions-mrna-covid-19-vaccines
- https://www.aaaai.org/conditions-and-treatments/library/asthma-library/covid19-vaccine
- https://community.kidswithfoodallergies.org/blog/covid-19-vaccine-information-for-people-with-food-allergies



